Last Updated on June 4, 2025 6:08 pm by INDIAN AWAAZ
By SHOBHA SHUKLA
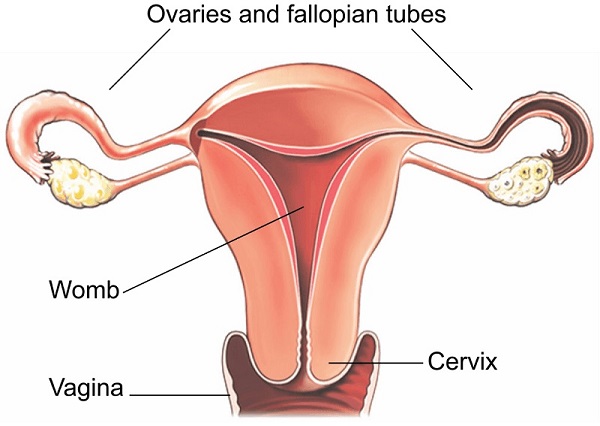
Cervical cancer remains a significant global health challenge, despite being one of the most preventable and treatable forms of cancer. According to the World Health Organization (WHO), it was the fourth most common cancer among women in 2022, affecting 660,000 women and resulting in 350,000 deaths worldwide. The tragedy lies in the fact that most of these deaths could have been avoided with timely vaccination, screening, and treatment.
The Disproportionate Burden on the Global South
A striking feature of cervical cancer is the disproportionate impact it has on women in low- and middle-income countries. In 2022, 94% of cervical cancer deaths occurred in these regions. India and China alone accounted for 42% of the global burden—India reported over 123,000 new cases and nearly 77,000 deaths, the highest in the world. The lack of access to preventive measures such as HPV vaccination and effective screening tools underscores a glaring inequity in healthcare access.
Women living with HIV are especially vulnerable, with a sixfold higher risk of developing cervical cancer. This puts a significant number of women at double jeopardy, particularly in countries like India where both HIV and cervical cancer rates are high.
A Call to Eliminate Cervical Cancer by 2030
Recognizing the preventable nature of this disease, WHO initiated a global strategy in 2018 aiming to eliminate cervical cancer by 2030. This strategy, endorsed by all governments, hinges on achieving three primary targets: vaccinating 90% of girls by age 15, screening 70% of women with high-performance tests by age 35 and 45, and ensuring 90% of women with pre-cancer or cancer receive appropriate care. However, the world is significantly off track to meet these goals by 2025.
Technology and Innovation: A Glimmer of Hope
Until recently, HPV vaccines like Gardasil and Cervarix, developed in wealthier nations, had limited reach in the Global South due to high costs and logistical hurdles. But a significant breakthrough came in 2022 when India’s Serum Institute, in collaboration with the government, developed Cervavac, the country’s first indigenous HPV vaccine. Despite this progress, the vaccine is not yet integrated into India’s public health system, slowing its widespread adoption.
In terms of diagnostics, traditional screening methods like Pap smears and visual inspection with acetic acid (VIA) are still prevalent in many low-resource settings. These methods, however, have limitations in sensitivity and require specialized infrastructure. Advanced molecular testing offers a more reliable alternative but has been largely inaccessible in rural or underserved areas.
That gap is now being addressed by innovations like India’s Truenat HPV-HR Plus test—a portable, battery-operated, RT-PCR-based molecular test capable of detecting eight high-risk HPV genotypes. Developed by Molbio Diagnostics, the Truenat platform can provide accurate results within an hour and has already been validated by multiple Indian research institutions in collaboration with WHO’s International Agency for Research on Cancer (IARC).
This test not only matches global standards in accuracy (100% sensitivity and specificity) but is also designed for deployment in remote areas, thanks to its portability, ease of use, and solar-powered operation.
A Community-Centered Approach
Community leaders and healthcare advocates stress that the fight against cervical cancer must be people-centered. Networks like the National Coalition of People Living with HIV in India (NCPI Plus) are actively working to raise awareness and integrate cancer screening into existing healthcare services for HIV-positive women. As women with HIV are more susceptible to cervical cancer, community engagement is vital to driving early detection and prevention efforts.
Pooja Mishra of NCPI Plus underscores the urgency of educating young people about HPV and the importance of vaccination and screening. According to her, it’s unacceptable that a disease both curable and preventable still claims so many lives.
Towards Gender-Neutral Prevention
HPV is not just a threat to women—it causes other cancers too, including those of the anus, penis, vulva, and oropharynx. Experts like Dr. Ishwar Gilada and Dr. Kuldeep Singh Sachdeva are calling for gender-neutral vaccination policies, noting that everyone at risk should be protected, regardless of gender.
HPV is primarily transmitted through sexual contact, including vaginal, anal, and oral sex, as well as skin-to-skin contact. This highlights the importance of educating the public on safe practices and the role of early vaccination, ideally before sexual debut.
The Road Ahead
Eliminating cervical cancer is possible, but only with a robust, equitable, and science-driven public health approach. Tools like Truenat HPV-HR Plus and Cervavac must be fully integrated into national health systems. More importantly, the focus must shift to ensuring these tools reach those who need them most—women in rural, marginalized, and resource-limited settings.
One death from cervical cancer is one too many. The technology exists. The knowledge exists. What remains is the political will and collective action to make cervical cancer a thing of the past.
– CNS
