Last Updated on March 19, 2025 6:19 pm by INDIAN AWAAZ
Dr. Manish Bhatnagar
Acute pancreatitis (AP) presents a multifaceted challenge in healthcare, demanding immediate medical attention and a multidisciplinary approach for effective pain relief, complication management, and prevention of prolonged residence. Incidences of AP vary between 4.9 and 73.4 cases per 100,000 worldwide.
When diagnosing acute pancreatitis, we look for at least two key features: abdominal pain consistent with the condition, serum lipase or amylase activity three times the upper limit of normal, and characteristic findings on imaging, typically through CT. Alcohol and gallstones dominate as etiological factors, but other rare causes include hypercalcemia, hypertriglyceridemia, drugs, malignancy, developmental anomalies, and genetic predisposition. The mortality rate for acute pancreatitis ranges from 3 to 17 percent, and differentiation between interstitial and necrotizing pancreatitis is crucial.
Moving on to severity assessment, the revised Atlanta definition categorizes pancreatitis into interstitial and necrotizing types. Severity is graded as mild (absence of organ failure), moderately severe (transient organ failure or local/systemic complications resolving within 48 hours), and severe (persistent organ failure with associated morbidity and mortality). Persistent systemic inflammatory response syndrome (SIRS) criteria aid in identifying severe cases.
Assessment of the severity of acute pancreatitis includes patient characteristics, altered mental status, comorbid disease, and SIRIS. Persistent SIRIS is associated with a mortality of 25% compared with 8% for transient SIRIS.
Laboratory findings such as BUN, hematocrit, and creatinine, along with clinical parameters like age, BMI, and comorbidities, contribute to severity assessment. The presence of persistent SIRS 48 hours post-admission is a strong indicator of severe acute pancreatitis. Also, radiology findings might include pleural effusions, pulmonary infiltrates, and multiple or extensive extrapancreatic collections.
Fluid resuscitation is a primary intervention in acute pancreatitis, and the approach has evolved to focus on goal-directed fluid administration while avoiding fluid overload. Nutritional support, preferably enteral, is initiated early. Other nutritional supports include initiation with a low fat solid diet as safe as liquid diet, Nasagastric vs Nasojejunal feeding, continuous slow feeding instead of bolus feeding.
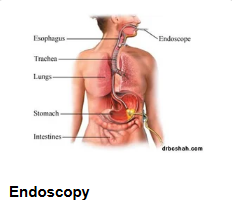
Urgent Endoscopic Retrograde Cholangiopancreatography (ERCP) is considered in cases of cholangitis, while antibiotics are reserved for suspected infections. Intra-abdominal hypertension (IAH) and compartment syndrome necessitate vigilant monitoring and potential interventions.
IAH is graded as follows: grade I (Intra-abdominal pressure 12-15 mmHg), Grade II (16-20 mmHg), Grade III (21-25 mmHg), grade IV (more than 25 mmHg).
Medical Interventions are necessary to decrease IAP and maintain abdominal perfusion pressure above 60mm/Hg. Hallow-viscera volume, nasogastric drainage, and rectal tubes can be used if endoscopic decompression is necessary. Surgical procedures include decompressive laparotomy and temporary abdominal closure.
Pancreatic necrosis, pseudocysts, and walled-off pancreatic necrosis are complications that may arise, each demanding tailored management approaches. Intervention timing for pancreatic necrosis is crucial, and a step-up approach involving minimally invasive techniques has gained preference over immediate surgery. Infections are addressed with antibiotics, while non-infected cases may undergo conservative treatment.
Minimally invasive treatment of pancreatic necrosis includes Laparoscopic surgery, percutaneous or radiological catheter drainage, video-assisted (VARD) or small incision-based retroperitoneal debridement, endoscopic necrosectomy, or combined modality treatment.
Carbapenems remain the first choice of antibiotics for treating infected necrosis; Procalcitonin may be used as guidance when antibiotic therapy is considered to reduce unnecessary antibiotic use. Neostigmine treatment should be considered for patients admitted to ICU with intra-abdominal hypertension. Patients with biliary necrotizing pancreatitis should be closely monitored following discharge and offered cholecystectomy when collections have been resolved.
To conclude, acute pancreatitis requires a comprehensive approach from admission to follow-up, including timely interventions based on severity assessments, fluid resuscitation, nutritional support, and management of complications. The evolving landscape of pancreatitis management emphasizes a nuanced and patient-centered approach.
Dr. Manish Bhatnagar is Consultant Gastroenterologist, Hepatologist & Therapeutic Endoscopist, Director & HOD, Gastroenterology, Orchid Mediservices, Ahmedabad
